By Maggie Jalowsky, Sick Cells and Jennifer Bright, Innovation and Value Initiative
Patient Engagement Gains Traction
Patient engagement in healthcare research is having a moment. Conferences, public policies, and thought leaders have finally begun to echo what so many of us have said for decades – patients, with all their rich complexities, must be at the center of healthcare research as full partners. And, healthcare research and value assessment must find ways to reduce health inequity, not exacerbate it.
Through a shared urgency to identify and test new scientific approaches, the Innovation and Value Initiative (IVI) and Sick Cells are collaborating on numerous initiatives to ensure that we ask the research questions that matter the most to people living with serious health conditions. In March, IVI released a proceedings report from its 2021 Methods Summit.[1]The 2021 IVI Methods Summit was partially sponsored by a Eugene Washington PCORI Engagement Award (EAIN-21256). The recommendations, developed in partnership with stakeholders across the healthcare industry, including leaders from Sick Cells, centered on ensuring that patient-centered impacts become central to research, policy, and practice.
Although there have been decades of hand-wringing about the need for patient-centered research with little effect, our two organizations see bright spots that suggest that we are finally moving in the right direction. We see examples of where organizations are working to move past the rhetoric of diversity, inclusion, and patient partnership to actually shift practices that we hope will lead to better outcomes and advance health equity across the healthcare system. Clearly, inertia abounds. And, the promise of value assessment is all too often used as a tactic to deny access to care. But, even as we remain clear-eyed about the challenges to changing the healthcare system, we believe it is also important to raise attention to the areas of potential as we work to ensure that patients are full partners in healthcare research.
Changing Policy Incentives
Many of the incentives in the U.S. healthcare system are not aligned to encourage collaboration, system change, or including patients as partners in healthcare research.[2]Bright, J. and A. Balch (March 1, 2022). Health Care Through the Lens of Patients’ Well-Being. Health Affairs Forefront Blog. Available: … Continue reading[3]Bright, J. Patient Value Is the Root of a Learning Health System. American Journal of Accountable Care. 2021;9(4):34-36. Available: https://doi.org/10.37765/ajac.2021.88805. Patient-centered research is not built into our system of work. We get it. Sometimes it is difficult to know where to start or the project may already feel too unwieldy. Data are not readily available, or may not represent diverse perspectives. Researchers may not know how to connect to patients and vice versa. Patients may be intimidated and may not know the jargon.[4]Sacristán, José A et al. “Patient involvement in clinical research: why, when, and how.” Patient preference and adherence. 2016;10:631-40. Available: … Continue reading
However, structural supports can move the needle. As IVI wrote earlier this year in our blog series, we were pleased to see ISPOR’s new Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) include both measures addressing health equity and patient engagement in the checklist for economic evaluations.[5]Husereau D, Drummond M, Augustovski F, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEER 2022) Explanation and Elaboration: A Report of the ISPOR CHEERS II Good Practices … Continue reading This is especially encouraging because the standards include both a patient engagement plan and an evaluation of engagement impact. Federal agencies, such as the U.S. Food and Drug Administration (FDA) and Centers for Medicaid and Medicare Services (CMS), have either already provided guidance documents on patient engagement or have established stronger requirements for patients to be included in both research and decision-making. The recently released CMS Framework for Health Equity will guide how the agency designs, implements, and operationalizes its policies and practices. Patient Centered Outcomes Research Institute (PCORI), which has funded projects with both our organizations, requires a patient and stakeholder engagement plan in all of its engagements and research awards. All of these point to examples where decision-makers are working to ensure that people with lived experience, especially those that are often lost in the healthcare system, are the focus.
Recent research[6]Frosch, D.L. From the Editor’s Desk: The Evolving Journey of Engaging Patients as Research Partners. J Gen Intern Med. 2022;37:1-2. Available: https://doi.org/10.1007/s11606-021-07315-1.[7]Xie RZ, Malik E deFur, Linthicum MT, Bright JL. “Putting Stakeholder Engagement at the Center of Health Economic Modeling for Health Technology Assessment in the United States.” … Continue reading has found that including people with lived experience from the outset of research projects does change the approach and increases the relevance of that research to patients. We see a need for these initial steps to go further, and to establish real financial incentives and research practices that ensure that people with lived experience are co-creators in the research process.
Testing New Methods
Both Sick Cells and IVI know that the devil is in the details when it comes to healthcare research – what research questions we ask, what data sets are available, and who to include in both leading and participating in t he research – can impact the outcomes. Sick Cells was recently awarded a Eugene Washington PCORI Engagement Award to examine the methods needed in healthcare research to incorporate principles of equity. We are bringing together experts from across the field to test how representativeness is measured for sickle cell disease. In preparation for this project, IVI and Sick Cells are collaborating on a series of research reports that highlight exactly how common assumptions in value assessment can lead to harmful conclusions for sickle cell disease.
IVI is also developing a model on major depressive disorder (MDD), and will include individual level measures, including race, gender, and socio-economic status to develop a more nuanced understanding of value. In a parallel study in collaboration with the University of Maryland PAVE Center, we are conducting a discrete choice experiment to better understand how people living with MDD make trade-offs regarding their care. The researchers focused their recruitment on populations often missed in this kind of research and are exploring the implications of the findings on value assessment. These choices may help provide the context to improve patient-centered value assessment.[8]“Health Technology Assessment: Evidence Generation Methods For Patient-Driven Values.” Health Affairs Forefront Blog. March 14, 2022. Available: … Continue reading
We hope this attention to details in the methods can begin to shift approaches from an item to cross off a checklist towards an active and valued relationship to ensure that research and value assessments are tailored to those they impact.
Building Partnerships and Common Ground
Our joint collaborations have highlighted that including patients as full co-creators of healthcare research shifts the tenor and approach of the research endeavor. It brings nuance and the willingness to acknowledge complexities in living with a serious health condition. It is only with these strong partnerships and engagement that it is possible to accelerate the goal of health equity.[9]Organizing Committee for Assessing Meaningful Community Engagement in Health & Health Care Programs & Policies. Assessing Meaningful Community Engagement: A Conceptual Model to Advance Health … Continue reading In IVI’s recently released report on rheumatoid arthritis, conversations with our patient co-authors emphasized that the “cost” of serious health conditions and related treatments is far more than just co-pays, but includes career disruption, transportation costs, having to adjust housing to accommodate mobility, as well as the cost of time navigating our complex healthcare system for both people living with the health condition and their caregivers.[10]Courtnay, C., Phillips, L., Masco, R., O’Hara Levi, S., Bright, J., Eller, J., Hyde, A., Kelly, M. and E. Malik. “First-Hand Perspectives in Rheumatoid Arthritis: Insights to Improve … Continue reading
Both of our organizations see partnerships across stakeholder groups as key to ensuring that change gain traction and to push the envelope in developing innovative solutions that are relevant to multiple perspectives. IVI’s recently launched Health Equity Initiative builds on the recommendations of the Methods Summit proceedings report with a cross-perspective challenge to identify better methods in value assessment.
We are pleased to see a growing number of perspectives t the table, but more needs to be done to make equity a central focus of these partnerships.
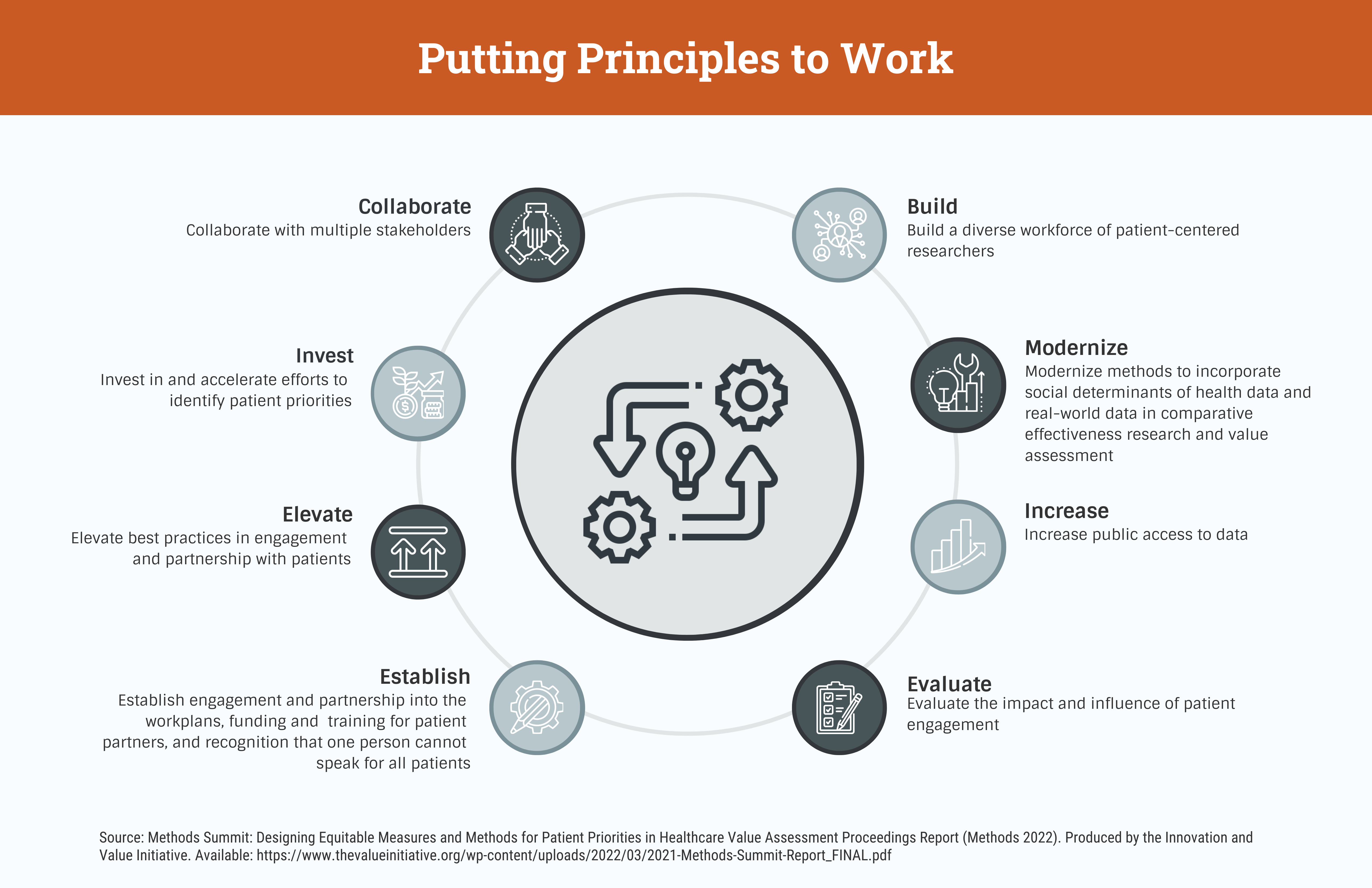
Put Principles to Work
IVI’s Methods Summit, supported trough a Eugene Washington PCORI Engagement Award (EAIN-21156) identified meaningful principles for changing our approach to comparative effectiveness research and value assessment. We are now at a point where we need more than principles but must lead with action to drive innovation in the healthcare system and reach continuum. While we do see shifts in public policy, new research initiatives, and a growing willingness to partner across perspectives, these are clearly early actions. To truly bring patients into value assessment and healthcare research, there will need to be a realignment of incentives to require the inclusion of patients as co-creators in research and investment in patient organizations to ensure they have the capacity to take on this critical role.
Invest in Patient Leadership
Over the past three decades, patient organizations have grown in their sophistication and capacity to collect real world data and conduct their own healthcare research to answer the questions that matter to them. Yet, patient organizations should not have the full burden of doing this work. Too often, patient organizations have had to scrounge for scarce resources just to gain a seat at the table or do the work themselves (Sick Cells, EveryLife Foundation, the Arthritis Foundation, the Alliance for Aging Research, the SynGAP Research Fund, National Health Council, and the list goes on). When patient organizations do conduct their own research, the findings are often dismissed as biased or not made available to decision-makers. IVI’s Methods Summit also highlighted the importance of reducing barriers to open access publishing of research – this is how patient organizations who conduct their own studies can gain attention and validity.
Build Capacity
As efforts to partner with patients increase, we also need to ensure that patients have the skills and understanding of the research process to collaborate as equal partners and researchers need the training in best practices in collaborating with patients. As IVI stated in its public comments to the Agency for Healthcare Research and Quality (AHRQ) earlier this spring,[11]Public comments submitted to ICER on its draft COVID-19 Report. Innovation and Value Initiative. March 2022. Available: … Continue reading this agency is in a unique position to invest in training for both patients and researchers, and offer a collaborative approach with other experts in the field to build the capacity of multiple stakeholders.
Conclusion
We are seeing a growing number of initiatives and policies that are working to ensure that patients are true partners in healthcare research – including new requirements for patient engagement, measures to assess the impact of that engagement, and a growing recognition that patients have a rich complexity that must be accounted for. We also know there is much work to be done and that all of us need to improve both our approach and strategies. Real change is time intensive and messy, and will require a willingness to change course as we aim towards a truly patient-driven healthcare system. Let the work begin.
About IVI
The Innovation and Value Initiative is a 501(c)(3) nonprofit research organization committed to advancing the science, practice, and use of value assessment in healthcare through collaboration among thought leaders in academia, patient organizations, payers, life science firms, providers, delivery systems and other organizations.
If you enjoy reading our blog posts and interested in learning more about IVI or becoming a member, please contact Erica Malik at jessica.brown@thevalueinitiative.org.
You can also find information on our membership webpage.
References[+]
| ↑1 | The 2021 IVI Methods Summit was partially sponsored by a Eugene Washington PCORI Engagement Award (EAIN-21256). |
|---|---|
| ↑2 | Bright, J. and A. Balch (March 1, 2022). Health Care Through the Lens of Patients’ Well-Being. Health Affairs Forefront Blog. Available: https://www.healthaffairs.org/do/10.1377/forefront.20220228.656900. (Final piece in 11-part series. |
| ↑3 | Bright, J. Patient Value Is the Root of a Learning Health System. American Journal of Accountable Care. 2021;9(4):34-36. Available: https://doi.org/10.37765/ajac.2021.88805. |
| ↑4 | Sacristán, José A et al. “Patient involvement in clinical research: why, when, and how.” Patient preference and adherence. 2016;10:631-40. Available: https://doi.org/10.2147/ppa.S104259. |
| ↑5 | Husereau D, Drummond M, Augustovski F, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEER 2022) Explanation and Elaboration: A Report of the ISPOR CHEERS II Good Practices Task Force. Value in Health. 2022;25(1):10-31. |
| ↑6 | Frosch, D.L. From the Editor’s Desk: The Evolving Journey of Engaging Patients as Research Partners. J Gen Intern Med. 2022;37:1-2. Available: https://doi.org/10.1007/s11606-021-07315-1. |
| ↑7 | Xie RZ, Malik E deFur, Linthicum MT, Bright JL. “Putting Stakeholder Engagement at the Center of Health Economic Modeling for Health Technology Assessment in the United States.” PharmacoEconomics. 2021;39(6):631-638. Available: https://link.springer.com/article/10.1007/s40273-021-01036-3. |
| ↑8 | “Health Technology Assessment: Evidence Generation Methods For Patient-Driven Values.” Health Affairs Forefront Blog. March 14, 2022. Available: https://doi.org/10.1377/forefront.20220311.897007. |
| ↑9 | Organizing Committee for Assessing Meaningful Community Engagement in Health & Health Care Programs & Policies. Assessing Meaningful Community Engagement: A Conceptual Model to Advance Health Equity through Transformed Systems for Health. NAM Perspectives. 2022. Commentary, National Academy of Medicine, Washington, DC. Available: https://doi.org/10.31478/202202c. |
| ↑10 | Courtnay, C., Phillips, L., Masco, R., O’Hara Levi, S., Bright, J., Eller, J., Hyde, A., Kelly, M. and E. Malik. “First-Hand Perspectives in Rheumatoid Arthritis: Insights to Improve Healthcare Research & Value Assessment.” Produced by the Innovation and Value Initiative. October 2021. Available: http://valueresearch.org/wp-content/uploads/2021/10/First-Hand-Perspectives-in-Rheumatoid-Arthritis_FINAL.pdf. |
| ↑11 | Public comments submitted to ICER on its draft COVID-19 Report. Innovation and Value Initiative. March 2022. Available: http://valueresearch.org/press-release-ivi-submits-comments-to-icer-draft-covid-19-report/. |