 In 2021, the Innovation and Value Initiative (IVI) and the Arthritis Foundation published a report, First Hand Perspectives in Rheumatoid Arthritis, describing how researchers often miss the priorities and needs of people living with rheumatoid arthritis (RA). Each of the patient-advocate co-authors reiterated that the costs related to RA reach far beyond direct medical costs, such as co-payments and deductibles. RA is a long-term, chronic illness. While some people manage their pain through medication many live with the lifelong question of when their treatments will stop working.
In 2021, the Innovation and Value Initiative (IVI) and the Arthritis Foundation published a report, First Hand Perspectives in Rheumatoid Arthritis, describing how researchers often miss the priorities and needs of people living with rheumatoid arthritis (RA). Each of the patient-advocate co-authors reiterated that the costs related to RA reach far beyond direct medical costs, such as co-payments and deductibles. RA is a long-term, chronic illness. While some people manage their pain through medication many live with the lifelong question of when their treatments will stop working.
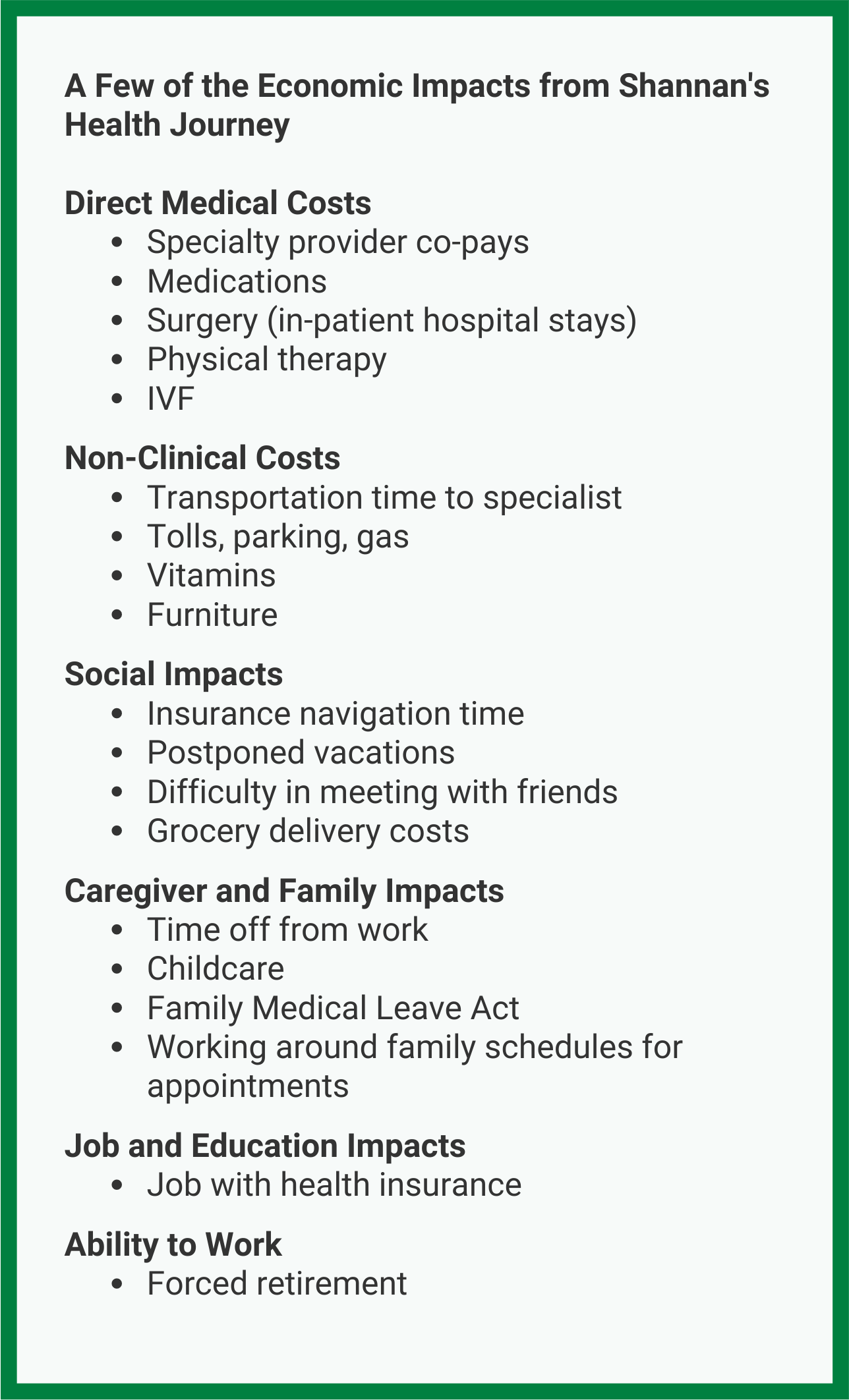
We invited one of our co-authors, Ms. Shannan O’Hara-Levi, to describe her recent “flare-up,” or significant spike in symptoms, to help illustrate the range of economic impacts people with serious health conditions might experience.
Shannan, thank you so much for joining me today. Can you share with us the background of your medical history to provide some context for your most recent health episode?
I was first diagnosed with juvenile rheumatoid arthritis at age three. Looking back, I first started showing symptoms, such as patting my knees to indicate pain and unwillingness to crawl, before I was one years old. It was in the 1980s, before many of the current treatment options were available and doctors thought I would be in a wheelchair before kindergarten. While careful attention, including many visits to physical therapists and occupational therapists, helped me avoid mobility devices, I’ve never experienced full remission.
In college, I chose a career path as a social worker for two reasons. First, I would be able to secure good health insurance and secondly this was a job I could management with my physical limitation. After seeing my parents spend hours navigating health insurance companies, I knew this would be in my future as well. For nearly a decade, I worked as a social worker, but after a bilateral shoulder replacement surgery in my early 30s, I was unable to return to work full-time.
Thank you, Shannan. Could you elaborate on the economic impacts of your most recent healthcare episode?
My husband and I were thrilled that I was able to give birth to our first child in January 2022. Although we had been trying to expand our family for many years, on and off due to my disease activity, we finally turned to fertility treatments and our baby was conceived during our initial round of IVF treatment. Due to the pregnancy, I had to change my medications and I committed to breastfeeding. My arthritis remained stable through the pregnancy, but my doctor warned me that the arthritis would likely flare up post-partum. By July, I knew the flare-up was coming, and as predicted, it was one of the worst episodes of my life. With no family nearby, we had to survive on our own.
Even with the medication increase, I had almost no relief, and could barely use my hands. My husband took time off from work through the Family Medical Leave Act to support me. My plans to visit family last summer were cancelled, and I couldn’t even have coffee with friends.
This disease is incredibly unpredictable. I never know how I will feel from one hour to the next.
We live outside of New York City and since June 2022, I have made 6-7 visits to my doctor’s office in the city. Keep in mind, a trip to see him takes at least half a day, and the parking and tolls cost nearly $100. While there are rheumatologists closer to me, I’ve been seeing him for more than eight years and it’s difficult to find a trustworthy doctor that also respects your treatment goals.
We’re still searching for an effective treatment, and I have tried four different biologics since September. Sometimes my doctor provides me with office samples to avoid going through a specialty pharmacy to get the biologics. On occasion, just waiting for the insurance approval can take up to six months. We are hopeful that this new regimen will work because the next level of treatment requires an infusion. My doctor’s infusion center is more than two hours away and the procedure takes nearly four hours – this is a full day lost, plus an additional day of recovery.
I’m in constant state of uncertainty – will this medication work? How long will it work? Will my insurance company cover the treatment if I am relying on samples right now?
I’m often reminded of when we scheduled my shoulder replacement surgery. My husband and I both took time off from work, and we had the entire surgery and recovery planned – meals, pet sitting, etc. Three days before the surgery, we still had not received approval from the insurance company. We spent two of those three days on the phone with the insurance company only to discover that the approval was sitting on someone’s desk. The additional time and anxiety from that human error is difficult to grasp.
 Are there other costs that you think are often missed when people think about the economic impacts of RA?
Are there other costs that you think are often missed when people think about the economic impacts of RA?
Another reason I love my rheumatologist is that he treats me as a whole person. He recommends dietary supplements and vitamins, often they are not covered by insurance and are expensive – more than $50 per bottle. We’re lucky because I can still navigate our house, but we did have to purchase a motorized stand-up recliner. It’s an ugly chair and costs anywhere between $600-$2,000, but sometimes it’s the only chair that works for me. My husband doesn’t have a work from home option, and we don’t have family nearby, so we schedule appointments when he is available for childcare. The other consideration for me with the baby is how to manage daily responsibilities and social activities. Even with the extra cost, I had groceries delivered long before the pandemic – carrying bags and putting everything away left me exhausted. And with the baby, it’s impossible.
Chronic pain also makes my mental functioning worse. Everyday activities are confusing and time consuming. The constant undercurrent of discomfort is a burden and it’s difficult to calculate the full impacts of this condition.
On many levels we are lucky – my husband has health insurance, we have a beautiful daughter, and I have a physician who has my trust. However, the economic impacts of my disease have grown over time – I had to stop working and we lost extra income, I struggle to find an effective treatment, we continuously visit the doctor to navigate insurance, and the rising costs of everyday items means we must thread the financial needle.
Thank you, Shannan. We are deeply appreciative that you are willing to share your experiences with us. As we have heard from so many people, we need to start with journeys like yours to better capture the full economic impacts on people and caregivers.
With the support from a Patient Centered Outcomes Research Institute (PCORI) Eugene Washington Engagement Award (EASCS-24-274), IVI is currently working to develop a framework that will provide guidance on how to better capture a full range of economic impacts on people living with serious health conditions. On March 14, 2023, IVI held a webinar that highlighted the need to bring patients’ lived experience into research – as drivers of research questions and to understand how to capture the full economic impacts of disease. As we work towards a final publication, we are keeping stories like Shannan’s as a key point of reference to guide the framework and our approach to understanding the economic impacts on people and their families.
You can learn more about IVI’s initiative on our website here.
###
About IVI
The Innovation and Value Initiative (IVI) is a 501(c)(3) tax-exempt, non-profit research organization dedicated to advancing the science and improving the practice of health technology assessment through development of novel methods and the creation and application of enhanced health technology assessment models to support local decision-making needs in healthcare.
Contact: Smita Sanwardeker
Phone: 267.909.7661
E-Mail: smita.sanwardeker@thevalueinitiative.org
